Immunotherapy is a type of cancer treatment that helps your immune system to fight cancer, by improving the immune cells natural ability to target the cancer cells.
Immunotherapy treatments are drugs that reactivates a person’s immune system so it can track down and kill their own cancer cells.
The Clatterbridge Cancer Centre is one of the UK’s largest providers of immunotherapy.
We also have an award-winning specialist immuno-oncology team who developed a pioneering service caring for people who develop side-effects and complications from immunotherapy. They provide education and training for healthcare professionals from across the UK and beyond.
What we do
About immunotherapy
The immune system recognises dangerous organisms such as bacteria and attacks them, preventing them from causing harm. This process is called an immune response.
Because cancer cells often find ways to disguise themselves or mutate (change), the immune system does not always recognise them as dangerous.
Immunotherapy works by activating the immune system so it can recognise cancer cells and destroy them.
There are many different types of immunotherapy and new treatments are becoming available.
Immunotherapy might be given by itself or in combination with other cancer treatments such as chemotherapy, targeted therapies or radiotherapy.
Your treatment will vary depending on which immunotherapy drugs you are having.
Your treatment will be given by:
- Drip – where treatment in a bag is given through a tube into your body, usually into your arm. Sometimes this can take several hours
Immunotherapy alert card
Feeling unwell: side-effects and complications
Occasionally, the immune system responds in an uncontrolled way to immunotherapy – this can cause side-effects.
You might not get any side-effects – but if you do, it is important to report them immediately because you might need treatment to prevent the problem from becoming more serious.
Side-effects to look out for
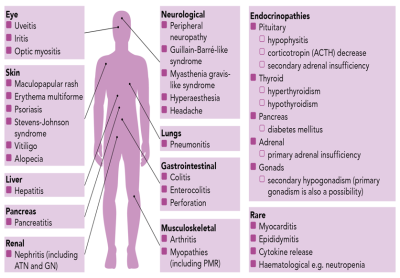
- Feeling more tired or confused
- Difficulty sleeping
- Feeling shivery or cold
- New or persistent headaches
- Feeling dizzy or light headed
- Change in your appetite
- Changes in your mood, feeling more anxious or irritable
- A loss or gain in weight
- Eyes become red or watery
- Pins and needles; leg weakness; issues with walking
- Feeling nauseous and/or vomiting (Very rare)
- An increase in bowel movement and/or diarrhoea. Any change in bowel habit should be taken seriously
- Blood, watery or foul smelling stools
- Cramping pains
- A new or worsening cough
- Changes in your breathing
- Feeling more short of breath
- A yellow tinge to your skin
- A skin rash or your skin is itchy
- May be confined to one area or all over your body
- Bleeding or bruising
- Sweating more than usual
- Muscle aches
- Severe or persistent muscle or joint pains
- Swelling to your legs
- Pain, weakness and/or paralysis in your arms and legs
- Some of the glands that produce hormones become inflamed e.g. Thyroid Gland
- This leads to the glands becoming underactive
- Hormone replacement therapy in the form of tablets may be required
- Glands will be checked regularly on blood test
General symptoms of gland issues may include:
- Lack of energy or motivation (fatigue)
- Muscle weakness
- Low mood
- Loss of appetite and unintentional weight loss
- Increased thirst
- Constipation
- Loss of libido (sex drive)
- Dry and scaly skin
- Brittle hair and nails
- Pain, numbness and a tingling sensation in the hand and fingers
- Sensitivity to cold
- Weight gain
Our team and locations
Your clinical team including your consultant and specialist nurses will look after your immunotherapy treatment. They will be there for you every step of the way. They will do all they can to support you and help with any questions you have.
Immunotherapy and other cancer drugs such as chemotherapy are known as systemic anti-cancer therapy (SACT).
Your immunotherapy will be given by our Chemotherapy and SACT team.
Our specialist Immuno-Oncology team provide advice and care for people who develop side-effects or complications from immunotherapy (known as ‘toxicities’).
They also run special clinics for patients with side-effects or complications from immunotherapy.
If you feel unwell while on immunotherapy, let your clinical team or our Hotline team (available 24 hours a day) know so we can adjust your care and help you stay well enough for your treatment. If needed, they can refer you to the Immuno-Oncology team.
The specialist Immuno-Oncology team deals with side-effects and complications (known as ‘toxicities’) from immunotherapy. The team includes clinical and non-clinical staff:
Consultant Medical Oncologist and Clinical Lead
Dr Laura Cossar
Immuno-Oncology Nurse Consultant and Lead Nurse
Trudy-Jane Guinan
Trudy provides leadership and clinical supervision and is responsible for developing the service. She also sees and treats patients referred to the service as outpatients or on our inpatient wards. She can prescribe medication.
Immunotherapy Service Manager and Clinical Nurse Specialist
Mark Toner
Immunotherapy Advanced Nurse Practitioners (ANP)
Senior nurses who have completed additional training and can prescribe medication and review patients referred to the service.
Immunotherapy Clinical Nurse Specialists (CNS)
Specialist nurses who manage patients day to day, including phone calls, advice and care.
Immunotherapy Project Support Manager
Reviewing service data and activity, looking at how the service should develop and helping the team to deliver those developments.
Immunotherapy Service Coordinator
Support for the team including arranging multidisciplinary team (MDT) meetings, liaising with patients and GPs, and maintaining records.
Immunotherapy Clinical Support Worker
Making sure blood results and blood tests are in place for patients, supporting the immuno-oncology clinic and liaising with patients.
You will have your immunotherapy treatment at one of the following sites:
- Clatterbridge Cancer Centre – Liverpool (our main hospital)
- Clatterbridge Cancer Centre – Wirral
- Aintree University Hospital: Marina Dalglish Centre
- Halton Hospital: CanTreat
- Ormskirk Hospital
- St Helens Hospital: Lilac Centre
- Noble’s Hospital, Isle of Man
- Treatment at home or in the workplace through our Clatterbridge in the Community service
Before you start treatment, your doctor and your clinical team will explain what to expect – including the expected benefits and any potential risks. They will get your consent showing you agree to treatment. You will have blood tests and health checks before starting treatment and while you are on it.
You can find out more about this on our Chemotherapy (SACT) page. Systemic anti-cancer therapy (SACT) is a general term for cancer drugs such as immunotherapy and chemotherapy.
Further information
Our patient information leaflets
Infliximab - frequently asked questions
Skin care advice for people on immunotherapy treatment
Adrenal / pituitary insufficiency following cancer immunotherapy
Adrenal/Pituitary insufficiency following cancer immunotherapy - A patient quick reference guide