Lymphoma is a type of blood cancer of the white cells called lymphocytes.
It is the fifth most common type of cancer in the UK.
Our lymphoma team also manage chronic lymphocytic leukaemia (CLL), another blood cancer affecting lymphocytes.
This page includes general information about lymphoma and CLL. When you have read this page, you might also be interested in the following pages about specific types of lymphoma and CLL:
- Hodgkin lymphoma
- Non-Hodgkin lymphoma (high grade)
- Non-Hodgkin lymphoma (low grade)
- Chronic lymphocytic leukaemia (CLL)
- Skin (cutaneous) lymphoma
About lymphoma 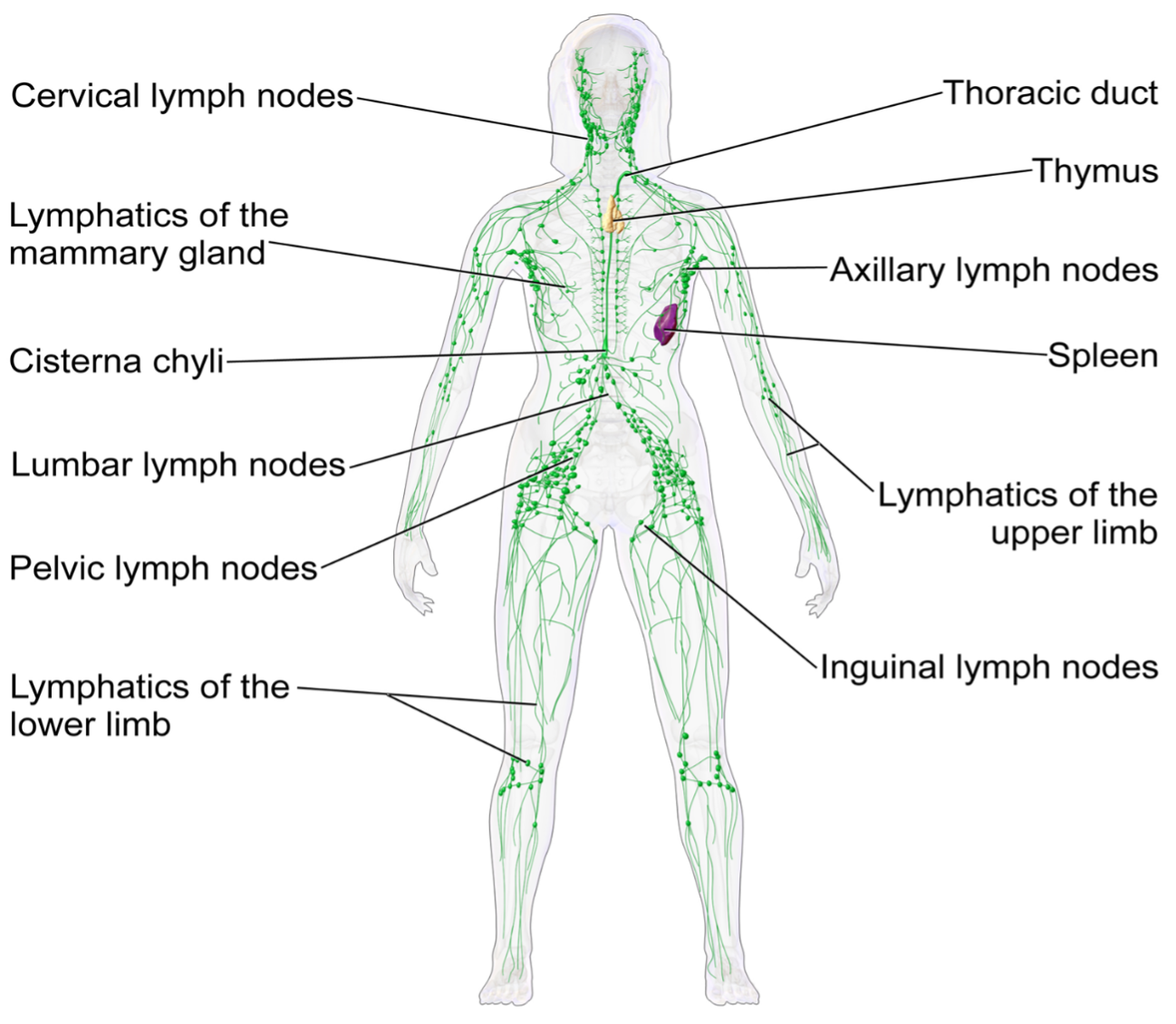
Lymphoma develops when lymphocytes grow out of control.
Lymphocytes are part of your immune system, which helps to fight infection.
Lymphocytes travel around your body in the blood and lymphatic system and pass through glands (lymph nodes), which are spread throughout your body. For this reason, lymphoma is also sometimes described as a cancer of the immune system.
There are many different types of lymphoma (over 60 types), but they are commonly grouped as:
- Lymphoma
- Hodgkin lymphoma
- Non-Hodgkin lymphoma
- Low grade ‘slow-growing’
- High grade
Risk factors for lymphoma include:
- Age – lymphoma is more common as people get older but Hodgkins lymphoma is more common in younger people (age 15-40)
- Family history – lymphoma is not inherited but the risk of developing it is slightly higher if you have a close relative with a blood cancer. The reasons for this are not clear
- Certain infections – lymphoma is not infectious but some viruses and bacteria are linked to an increased risk. These include Epstein-Barr virus and hepatitis C
- Lowered immune system – this includes people with HIV (human immunodeficiency virus) or who have had an organ or bone marrow transplant
- Autoimmune conditions – most people with autoimmune conditions do not develop lymphoma but you may be at slightly greater risk if you take immunosuppressive drugs because of them
Symptoms vary depending on the type of lymphoma and where it is in the body.
Many people have no symptoms. They might have swollen lymph nodes – small, painless lumps usually found in the neck, armpit or groin. Sometimes signs of lymphoma are only found during a routine blood test or a scan for something else.
Symptoms of lymphoma can include:
- Swollen lymph nodes that you can feel – small, painless bumps usually found in the neck, armpit or groin
- General symptoms (sometimes known as B symptoms)
- Unexplained weight loss
- Night sweats
- Fever
- Other non-specific symptoms:
- Fatigue
- Difficulty getting over infections
- Itching
- Anaemia
People can be referred to our lymphoma team by their GP or other healthcare professionals (including those in other hospitals).
The team sees people with symptoms that could be lymphoma as well as those diagnosed with lymphoma.
Being referred to the lymphoma team does not always mean you have cancer – you might be referred to them just because you have symptoms that need to be checked by a specialist. We will explain this to you at your appointment.
The only way to confirm if someone has lymphoma is to carry out a biopsy – a small sample of body tissue is removed and checked under a microscope.
Leukaemias including chronic lymphocytic leukaemia (CLL) can sometimes be diagnosed from blood tests.
When you are referred to the lymphoma, they might need to carry out a range of tests to:
- Diagnose if you have lymphoma (if you are referred with suspected lymphoma)
- Check if the cancer has spread and, if so, how far (staging the cancer)
These tests might include:
- Blood tests
- Scans including PET/CT, CT, ultrasound and MRI
- Biopsies
- Bone marrow biopsy
- Lumbar puncture
Treatment at The Clatterbridge Cancer Centre
Treatment depends on a range of factors including the type, size, stage and location of your tumour. It may also depend on your age, general health and genetic factors (linked to the DNA changes in your cells) that tell us how your cancer developed.
Treatment options can include one or more of the following:
- Active monitoring
- Drug therapies such as chemotherapy, endocrine therapy, targeted treatments, bispecific antibodies and immunotherapy. The general term for these is systemic anti-cancer therapy (SACT)
- Radiotherapy
- Cellular therapy (such as stem cell transplant and CAR-T therapy)
When you are diagnosed, your care will be discussed at a multidisciplinary team meeting (MDT) where different specialists will consider the best treatment options for you. Your doctor will discuss this with you so you can decide what is right for you.
Genomics is the study of a person’s genes (or ‘genome’) – the material in DNA that makes each person unique. Cancer is caused by changes in the DNA of a cell and tell it to multiply out of control.
Understanding where this change has occurred – for example, which gene is faulty – can help us know which treatment will give you the best chance of killing the cancer cells and stopping new ones from growing.
Your clinical team will explain this to you in more detail at your appointment.
We provide specialist care for lymphoma and chronic lymphocytic leukaemia (CLL).
Active monitoring / watch and wait
Some people with lymphoma or CLL do not need treatment straight away. Instead they have regular check-ups with our team to monitor their cancer (sometimes referred to as active monitoring or ‘watch and wait’).
This is quite common for low-grade (slow growing) lymphomas and CLL.
We might recommended this if there is no benefit to you in starting treatment before you need it.
It does not mean that there is no treatment available – it just means you can avoid treatment and its side-effects until you need it. Having treatment before you need it does not make you live longer. Treatment is just as effective when you do need it.
Having treatment
The anti-cancer treatments we offer for lymphoma and CLL include:
- Chemotherapy
- Radiotherapy
- Targeted treatments and antibody therapy
- Steroids
- Maintenance therapy
- Stem cell transplants (also known as bone marrow transplants) – Stem cell transplantation is a possible alternative if you do not respond to
- CAR-T cell therapy
- Clinical trials
Supportive treatment that helps with symptoms of lymphoma or side-effects from treatment is also important. This includes:
- Blood transfusions
- Growth factors
- Immunoglobulin replacement therapy
- Complementary therapy
- Treatment to control symptoms (palliative care)
Systemic anti-cancer therapy (SACT)
SACT is a term used to describe the different drug therapies for cancer. These include:
- Chemotherapy – which aims to kill cancer cells
- Immunotherapy – which aims to train your immune system to attack cancer
- Targeted therapies – which specifically target and interfere with processes inside cells that help cancers grow
- Antibody therapy – monoclonal antibodies are special medicines designed to recognise specific cancer cells and then destroy them. One of the most commonly used medicines is called rituximab
Steroids are used together with chemotherapy for some types of lymphoma because it can make treatment more effective.
Targeted therapies are new treatments that are specific for certain types of lymphoma. They often have fewer side-effects than chemotherapy.
Find out more about systemic anti-cancer therapy at The Clatterbridge Cancer Centre.
Radiotherapy
You might have radiotherapy as part of your lymphoma treatment for various reasons depending on:
- How big the lymphoma is
- What stage it is (whether it has spread)
- How you respond to chemotherapy
- Sometimes radiotherapy is given to help relieve symptoms
Find out more about radiotherapy at The Clatterbridge Cancer Centre.
Stem cell transplant (also known as bone marrow transplant)
Stem cell (bone marrow) transplantation is a possible alternative if you do not respond to treatment for lymphoma. For some patients, a transplant may offer the best chance of cure.
Find out more about stem cell transplants at The Clatterbridge Cancer Centre.
Research and trials of new cancer treatments are an important part of our work. Your consultant will tell you about any clinical trials that may be suitable for you.
You are also very welcome to ask us about clinical trials during your appointments. We will be happy to answer any questions you have.
Some of the services we provide include:
- A rapid diagnostic clinic for diagnosis of lymphoma and related cancers
- Clinics in Clatterbridge Cancer Centre – Liverpool (CCC-Liverpool) and Clatterbridge Cancer Centre – Aintree (CCC-Aintree)
- Outpatient chemotherapy in CCC-Liverpool and the Marina Dalglish Centre at Aintree University Hospital
- Inpatient care on Ward 4 and Ward 5 at CCC-Liverpool
- Blood cancer services to all acute hospitals in Liverpool
- Radiotherapy for lymphoma
- Regional support to haematology teams in Merseyside, Cheshire and North Wales
- Outreach services to the Isle of Man
- Clinical trials are delivered at CCC-Liverpool and CCC-Aintree
Our team is made up of the following members:
- Consultants
- Specialist Registrar
- Advanced Nurse Practitioner
- Clinical Nurse Specialists
- Research Nurses
- Pharmacist
- Consultant Clinical Scientist
- Pathway Coordinator
- Cancer support worker
Our operational management team and administrative support makes sure the service runs smoothly.
Consultants
These are the people you are most likely to meet when you come for your clinic appointment or on the inpatient ward.
Our consultants are experts in diagnosing and treating lymphoma and CLL. They will discuss your diagnosis and treatment options (if you need treatment) at all stages.
Many people will be eligible to take part in a research study or clinical trial. Your consultant will tell you if this is an option for you. Please tell us if you are interested in clinical trials.
Haemato-oncologists
- Dr Jeffery Smith, Consultant Haematologist and service lead
- Dr Arvind Arumainathan, Consultant Haematologist
- Prof Nagesh Kalakonda, Consultant Haematologist
- Prof Andrew Pettitt, Consultant Haematologist
- Dr Vikram Singh, Consultant Haematologist
- Dr Matthew Wells, Consultant Haematologist
- Dr Stella Williams, Consultant Haematologist
Other consultants
- Dr Rachel Brooker, Consultant Clinical Oncologist (specialist in radiotherapy)
- Dr Peter Robson, Consultant Clinical Oncologist (specialist in radiotherapy)
- Dr Richard Azurdia, Consultant Dermatologist (specialist in skin lymphoma)
Nurses
Clinical Nurse Specialists (CNS)
They are there to help and support you as well as coordinate your care in hospital and at home. Your CNS can help you to understand your cancer diagnosis and treatment options and support you through your cancer experience.
They can help with any problems or questions that you or your family might have. They might also see you in clinic for follow-up appointments.
Our clinical nurse specialists are:
- Lauren Burke
- Amy Towers
- Angela Foster
- Hayley Glover
- Jessica Jones
Advanced Nurse Practitioner (ANP)
An advanced nurse practitioner (ANP) is a senior specialist nurse. The ANP in Lymphoma and CLL is Chris Ward.
Research Nurse
If you are having your treatment as part of a clinical trial, one of our research nurses will act as your specialist nurse.
Our research nurses are:
- Jane Tinsley (Lead Research Nurse)
- Irwin Balquin
- Darren Keats
- Aimee Weatherall
Other team members
Consultant Clinical Scientist
Our consultant clinical scientist, Tracey Smith-Straney, has many years’ experience as a laboratory scientist specialising in blood cancer diagnosis. She is also fully qualified to manage blood cancer in clinical settings.
Senior Pharmacist
The senior pharmacist makes sure that any treatment or chemotherapy you receive is prescribed and administered correctly. You might have a telephone appointment with them when you are on active treatment. This is check that you are ready for your next treatment dose and are tolerating the treatment well. Our senior pharmacist is Aileen McCaughey.
Pathway Coordinator
Our pathway coordinator helps speed up and coordinate tests for new patients with suspected blood cancers (i.e. people without a previous diagnosis of blood cancer). Our pathway coordinator is Haydn Pidcock.
Patient Counsellor and Clinical Psychologists
Linda Boyne is the counsellor for patients with blood cancer.
There is a team of clinical psychologists who can offer more advanced psychological support. One of the team will suggest this to you if they feel it is in your best interests. You might then be referred to the psychology specialist team.
Cancer Support Worker (CSW)
The cancer support worker (CSW) works alongside the clinical nurse specialists to provide support and information to patients and families. Our CSW is Caron Plimley.
Further information
Our Cancer Information and Support Centres can provide individualised help and support for patients and families affected by cancer. The team’s main base is in Clatterbridge Cancer Centre – Liverpool but they also work at our Aintree and Wirral hospitals.
There are also local Macmillan services in other hospitals across our region.
External sites that offer extra support and information about different types of lymphoma include: