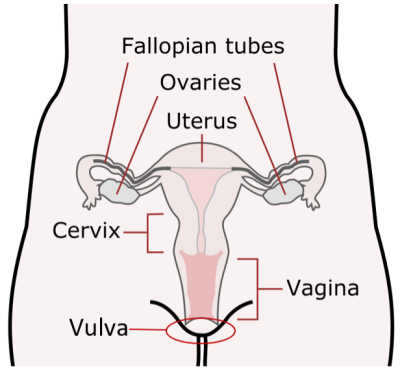
The vulva is a woman's external genitals. It includes:
- the lips surrounding the vagina (labia minora and labia majora)
- the clitoris, the sexual organ that helps women reach sexual climax
- the Bartholin's glands, 2 small glands each side of the vagina
Most of those affected by vulval cancer are older women over the age of 65.
The condition is rare in women under 50 who have not yet gone through the menopause.
About vulval cancer
The exact cause of vulval cancer is unclear, but your risk of developing the condition is increased by the following factors:
- Increasing age
- Vulval intraepithelial neoplasia (VIN) – where the cells in the vulva are abnormal and at risk of turning cancerous
- Persistent infection with certain versions of the human papillomavirus (HPV)
- Skin conditions affecting the vulva, such as lichen sclerosus
- Smoking
You may be able to reduce your risk of vulval cancer by stopping smoking and taking steps to reduce the chances of picking up an HPV infection.
- A persistent itch in the vulva
- Pain, soreness or tenderness in the vulva
- Raised and thickened patches of skin that can be red, white or dark
- A lump or wart-like growth on the vulva
- Bleeding from the vulva or blood-stained vaginal discharge between periods
- An open sore in the vulva
- A burning pain when peeing
- A mole on the vulva that changes shape or colour
Treatment depends on a range of factors including the size, stage and location of your tumour. It may also depend on your age, general health and genetic factors (linked to the DNA changes in your cells) that tell us how your cancer developed.
Treatment options can include one or more of the following:
- Surgery – this may be before, during or after other treatments
- Drug therapies such as chemotherapy and immunotherapy. The general term for these is systemic anti-cancer therapies (SACT)
- Radiotherapy
When you are diagnosed, your care will be discussed at a multidisciplinary team meeting (MDT) where different specialists will consider the best treatment options for you. Your doctor will discuss this with you so you can decide what is right for you.
Genomics and cancer
Genomics is the study of a person’s genes (or ‘genome’) – the material in DNA that makes each person unique. Cancer is caused by changes in the DNA of a cell and tell it to multiply out of control.
Understanding where this change has occurred – for example, which gene is faulty – can help us know which treatment will give you the best chance of killing the cancer cells and stopping new ones from growing.
If gene testing can be used and if this is recommended for you, your clinical team will explain this to you in more detail at your appointment.
Our treatments
At The Clatterbridge Cancer Centre, we provide specialist non-surgical treatment for vulval cancer. We also work closely with surgical teams in other hospitals to plan and coordinate your care every step of the way.
Systemic anti-cancer therapy (SACT)
SACT is a term used to describe the different drug therapies for cancer. These include:
- Chemotherapy – which aims to kill cancer cells
- Immunotherapy – which aims to train your immune system to attack cancer
Chemotherapy
Chemotherapy is a drug that is used to kill cancer cells or stops them from dividing and multiplying. It can be used alone, with surgery and/or radiotherapy, with hormonal therapy, or other anti-cancer drugs such as targeted or biological therapies.
You may have chemotherapy for vulval cancer:
- After surgery to help stop the cancer coming back
- Alongside, before or after radiotherapy
- To help slow the cancer down and ease symptoms if it has spread to other parts of your body
Radiotherapy
Radiotherapy involves using high-energy radiation to destroy cancerous cells. It is usually given in combination with chemotherapy, this is called chemo radiation.
There are several ways it can be used to treat vulval cancer:
- Before surgery to try to shrink a large cancer – this is to help make the operation possible without removing nearby organs
- After surgery to destroy any cancerous cells that may be left – for example, for cases where cancer cells have spread to the lymph nodes in the groin
- As an alternative to surgery, if you're not well enough to have an operation
- To relieve symptoms in cases where a complete cure is not possible – this is known as palliative radiotherapy
The radiotherapy treatments we offer for vulval cancer include:
- Traditional external beam radiotherapy – where radiation is delivered from outside the body
Clinical trials
Research and trials of new cancer treatments are an important part of our work. Your consultant will tell you about any clinical trials that may be suitable for you.
You are also very welcome to ask us about clinical trials during your appointments. We will be happy to answer any questions you have.
Find out more about clinical trials.
Treatment locations
We have a multi-site model where we visit hospitals across Cheshire and Merseyside to provide treatment and consultations closer to patients’ homes.
We provide systemic anti-cancer therapies (e.g. chemotherapy and immunotherapy) for cervical cancer at the following sites:
- Clatterbridge Cancer Centre – Liverpool
- Clatterbridge Cancer Centre – Wirral
- Halton – CanTreat Unit
- St Helens – Lilac Centre
- Outreach services to the Isle of Man
We provide radiotherapy for vulval cancer in one of our three specialist sites:
Clinical trials for vulval cancer are delivered at Clatterbridge Cancer Centre – Liverpool.
We have a multi-site model where we visit hospitals across Cheshire and Merseyside to provide treatment and consultations closer to patients’ homes.
We provide systemic anti-cancer therapies (e.g. chemotherapy and immunotherapy) for cervical cancer at the following sites:
- Clatterbridge Cancer Centre – Liverpool
- Clatterbridge Cancer Centre – Wirral
- Halton – CanTreat Unit
- St Helens – Lilac Centre
- Outreach services to the Isle of Man
We provide radiotherapy for vulval cancer in one of our three specialist sites:
Clinical trials for vulval cancer are delivered at Clatterbridge Cancer Centre – Liverpool.
The team consists of clinical oncologists, medical oncologists, clinical nurse specialists, radiographers, pharmacy, research practitioners, administrative support and a cancer support worker.
Our operational management team makes sure the service runs smoothly.
Medical Oncologists
- Dr Rosie Lord
- Dr Danielle Shaw
- Dr Laura Cossar
Clinical Oncologists
- Dr Karen Whitmarsh
- Dr Anthea Cree
- Dr Elizabeth Mullen
Associate Specialist Doctor
- Dr Mona Chopra
Specialist Doctor
- Dr Muhammad Heiba
Clinical Nurse Specialists
- Caron Robb
- Jenny Gleave
Cancer Support Workers
- Rachel Burns
Brachytherapy Clinical specialist
- Sarah Stead
Chemotherapy at The Clatterbridge Cancer Centre
Immunotherapy at The Clatterbridge Cancer Centre
Radiotherapy at The Clatterbridge Cancer Centre
Our Cancer Information and Support Centres can provide individualised help and support for patients and families affected by cancer. The team’s main base is in Clatterbridge Cancer Centre – Liverpool but they also work at our Aintree and Wirral hospitals.
There are also local Macmillan services in other hospitals across our region.
External sites that offer extra support and information about vulval cancer include: